- Sol Wellness
- Mar, 06, 2017
- Inflammation, Nutrition, Patient Education, Tissue Healing
- Comments Off on Low-Grade Inflammation and Musculoskeletal Diseases
LOW-GRADE INFLAMMATION AND MUSCULOSKELETAL DISEASES
Let’s talk about what Low-grade inflammation is, what kind of diseases low-grade inflammation could be linked to, and the principles for the lifestyle and habits that can relieve and/or prevent low-grade inflammation. Many musculoskeletal diseases like osteoarthritis and back problems can be partly linked to low-grade inflammation and much of this condition can be controlled with lifestyle choices. In the viewpoint of naprapathy this is quite interesting as we deal with these musculoskeletal problems. There is quite a lot of scientific research on this subject and some promising evidence based on these scientific studies supporting dietary changes and their positive effects on inflammation and osteoarthritis.

What inflammation? Low-grade inflammation means a small but constant inflammatory state in the body. In this state inflammatory agents can be found if tested in a laboratory. Examples of these inflammatory agents include prostaglandins, tumor necrosis factor, free oxygen radicals, and bradykinin. These same inflammatory agents are secreted when there is a tissue injury for example a wound in a finger. When there is, for example, a wound in the finger, the inflammatory agents sensitize the pain receptors which makes you to guard the site of the injury and like this enables the healing process to take place. If one would oversimplify things it would be easy to assume that if there is constantly these inflammatory agents during the low-grade inflammation, it would lead to chronic pain. Of course it’s quite naive to make straightforward conclusions like this because for instance the contents of the the inflammatory agents are totally different in these two conditions. However, what we can do, is ask the question what if the low-grade inflammation is tolerated for longer period of time?
Inflammation – the two sides of the same coin. If we take a step back and try to figure out the beneficial aspects of the inflammatory reaction in the tissues and delve into the biological base of it we find that inflammation is actually natural and useful process in the body. The tissue injuries heal through a certain process that has different phases. Roughly, there are four phases. The first phase is coagulation. For example if there is a wound in a finger the blood starts to coagulate there. The second phase is a local inflammation in the wound area. In the third phase the cells start to proliferate and in the forth phase the remodeling of the injury area takes place through the production of scar tissue and new for example skin tissue. So no need to think inflammation is only a bad thing. It has many important implications in the body. The important thing to note is the timeline. Inflammation induced by a tissue injury in a healthy person resolves spontaneously during the injury healing process.
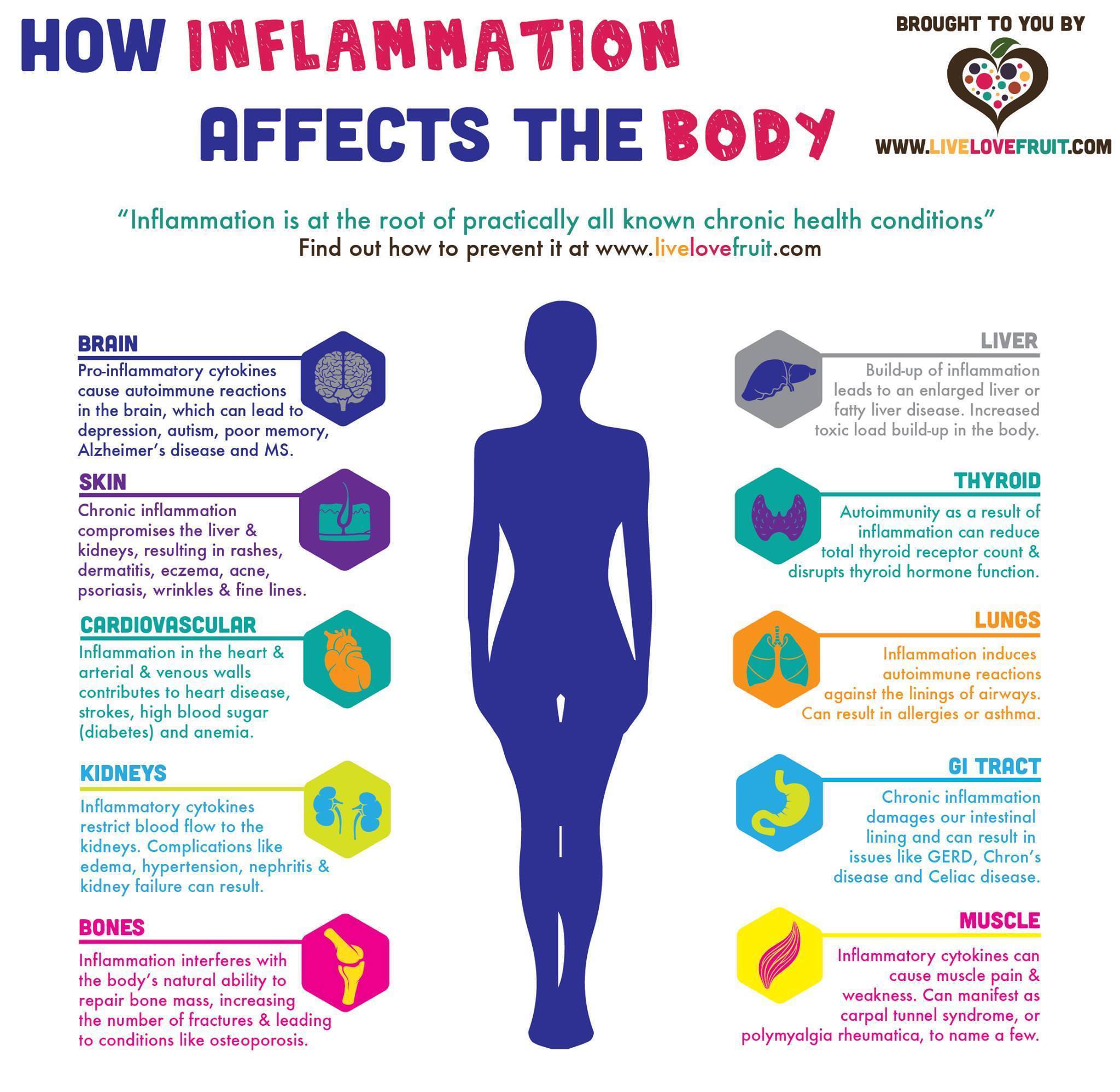
What if there are constantly inflammatory agents in the body? It has been proposed that this could predispose individuals to musculoskeletal pain for example osteoarthritis or rheumatoid arthritis. However, there is still a debate in the scientific research if the low-grade inflammation is a partial reason to osteoarthritis or whether low-grade inflammation is rather the consequence of the unfavorable stress to the joints. It has been also proposed that many inflammatory diseases could be partially linked to low-grade inflammation. These are for example Inflammatory Bowel Disease, Fibromyalgia, Type II Diabetes, Alzheimers Disease and Heart and Vascular Diseases.
The western lifestyle and diet predisposes us to low-grade inflammation. Low-grade inflammation can develop if the omega-3 and omega-6 ratio isn’t optimal and the diet is plain and contains a lot of processed foods and lacks vegetables and fruits. Also, a passive lifestyle, obesity, smoking and stress could be contributing factors to low-grade inflammation. This is not really new information. I’m sure most of us know already know this. It is certain that low-grade inflammation is one of those things you can really influence with your own lifestyle choices. To some of us this might be liberating but others might feel anxious. It’s liberating that you can be empowered to take control of your own health but on the other hand it can be challenging to change habits and this might make you feel anxious.
If the thought of changing habits makes you feel anxious, never fear, here is some practical advice considering lifestyle to alleviate or help prevent low-grade inflammation.
Here is how you can help your healing injury through eating the right foods.
Nutrition is important for survival we require it to be able to function in our daily lives. Sustaining an injury increases the physiological demand of our body to promote tissue repair. It is understood that optimizing nutrition can facilitate and expedite recovery times.
Now there is so much advice out there on nutrition, it can be very confusing for us to know what to eat, when to eat and why you should eat it. I personally would not get to caught up in the technicalities of it unless you are an elite athlete. There are plenty of agreements/disagreements out there about when to eat i.e. within 40 minutes post exercise, the use of protein supplements.
Let’s give you a quick low down on body make up and tissue repair. Soft tissues consist of collagen, elastin and ground substance surrounded by an extracellular matrix (a scaffold to hold everything together). Soft tissue such as tendons, ligaments, fascia, skin, fibrous tissues, fat, and synovial membranes are classed as connective tissue as they connect, separate or support different parts of the body. Muscle, nerves and blood vessels are separated by connective tissue in order to move and glide within the body. So knowing how are tissues a composed let’s have a closer look at the process of healing in order to understand how we can optimize each phase with appropriate nutrition.
Stages of healing
Tissue healing tends to come in 3 phases (if you exclude initial bleeding) an Inflammatory phase, a proliferation phase, and a remodeling phase. Depending on the type and severity of the injury will determine the length of time it takes for the injury to heal.
Inflammatory phase – The inflammatory response is necessary for proper healing. This stage may last for a few hours up to several days depending on the injury. Chemical mediators, cleaning cells, scaffolding cells and fluid come into the injury site to begin the cleaning and repair process. Often recommendations such as NSAIDs (ibuprofen) are made to decrease or even eliminate the inflammatory response. However, given that inflammation is a critical component of the healing process, elimination of the inflammation may not be ideal for optimal recovery. The processes associated with inflammation are energy requiring thus energy expenditure increases during wound healing.
Proliferation phase – The proliferation phase has a crossover period with inflammation. It begins within 24-48 hours but reaches its peak around 2-3 weeks. It is primarily associated with laying down of collagen (building cells slowly replace the scaffolding cells) for scar formation and proliferation of local fibroblasts. Simply put this is new tissue being laid down in a hap-hazard fashion to give the injury strength. Proliferation, as with inflammation, requires energy to promote the processes.
Remodeling phase – Remodeling has been shown to begin within the 1st week, and can last up to a year or longer dependent on the tissue state and severity of the injury and also how the tissue has been influenced. Yet remodeling is a continual process. You are constantly remodeling throughout your life. The repaired tissue that was formed by the first 2 phases gets replaced by type I collagen. It is suggested that the tissue is laid down in lines of tension.
A quick point I would like to make here that is very relevant to every phase is the process of optimal loading and mechanotherapy (movement progression). Studies have shown the benefits of exercise prescription in optimizing injury management and influencing tissue health. So keeping the injury immobilized for long periods of time is not ideal, which is why it is important to receive some kind of manual therapy or physical therapy soon after the injury.
So how do we optimize theses phases with nutrition?
We require certain percentages of macro-nutrients (water, carbohydrates, fats and proteins) and micro-nutrients (vitamins and minerals) in our diet during tissue healing.
Collagen is being replaced and replenished through protein synthesis and breakdown so it would make sense to increase your protein intake to aid with tissue recovery. Leucine in particular has been shown to enhance protein synthesis. It is found in a variety of food sources including soy beans, beef, eggs and also as a supplement in powder form.
As Sports Nutritionist Edel Keaveney explains,
Timing of protein is crucial for promoting muscle repair and growth. It is best to distribute protein evenly throughout the day rather than just consuming it in one or two meals. For sports people, it is recommended that 20-25g of protein is consumed with each main meal. People who are not exercising but need optimum dietary protein for repair of an injury would also benefit from spreading their protein intake evenly throughout the day.
Micro-nutrients such as vitamins A and C have been shown to have the most beneficial effect on tissue healing due to their direct interaction with collagen deposition and their effects on inflammation. Foods include fruit and vegetables such as avocado, oranges, bananas, garlic, green beans, broccoli and kale. These also have a high antioxidant content which add an anti-inflammatory effect.
Tissue healing requires energy
Depending on the injured limb you may have an increased demand on your energy intake. If you have injured a lower limb you may have a higher expenditure of energy if you are using crutches compared to a shoulder, elbow, or wrist injury where your energy expenditure will be lower. Carbohydrates and fats are our main energy producing food sources. They have been shown to be responsible for driving protein synthesis, thus complementing each other. If you have low energy levels then this can lead to impairing protein synthesis. It has been proposed that a fit athletic male uses 500kcal of energy a day on protein synthesis that’s without performing physical activity!
Additionally, Fat intake, particularly omega 3 fatty acids and monounsaturated fats, are most beneficial to promote tissue healing as they express anti-inflammatory and immuno-modulatory properties. Omega 3 and monounsaturated examples consist of flax seeds, salmon, avocado, sardines and everyone’s favorite the brussel sprout. A diet of processed food, fast food, microwave TV dinners, white bread, white rice, starchy potatoes, and pasta etc. can be high in carbohydrates causing an accumulation of visceral fat (the stuff that sits on your organs) and have been shown to have a pro-inflammatory effect. It’s a good idea to avoid those foods while recovering from an injury and they are empty calories with minimal nutrition. Imagine it similar to putting sugar in the gas tank of your car, eventually something is going to break under those conditions.
There are some differences of opinion around omega 6 fatty acids due to their pro-inflammatory effects. However, Omega 3 have been shown to have anti-inflammatory properties. The important take home message is that a balanced ratio of omega 3 and 6 support inflammation, as you need to have inflammation in order to promote healing and collagen deposition. It can be difficult to know how much of each we are consuming since omega 6s are in abundance in foods such as cooking oils and corn fed animals that give us our meat products. It is wise to know the source of your food and how it has been reared. I would suggest shopping for meat products at your local Co-op where you know the meat is local and grass-fed with no GMO’s or anti-biotics. Many packages at the grocery stores are misleading with the words “natural” or “healthy” on them. Also, cooking with coconut oil is the best option since vegetable oils have a lot of Omega 6s and oxidize with heat.
It is worth noting an increase in pro-inflammatory food sources such as omega 6s and 9s fatty acids, saturated fats, and high sugar content foods have been linked to cell wall breakdown leaving the cells open to free radicals which will weaken its structure and promote disease. It also increases pro-inflammatory cytokine production which can increase illness, tissue breakdown and delay healing. Meaning that we could be more prone to tendinopathy, weaker muscles, ligament injury etc. when we are not eating nutritious whole foods.
Other micro-nutrients including copper, iron, magnesium and zinc in fruits and vegetables support tissue regeneration and repair as they help to support early inflammation, reverse post-injury immune suppression, assist in collagen formation, strengthen connective tissue, as well as support protein synthesis. Effectively your diet will have an affect throughout all the stages of tissue healing. If you balance it well or increase your intake of macro and micro-nutrients slightly this will help to optimize tissue repair, dependent on the location, severity and duration of the injury.
Summing up it is important to make sure that you are not malnourished as this will delay wound healing. Eating processed food that are high in trans-fats and saturated fats will have an adverse affect on tissue repair/wound healing. Depending on your fitness levels and determination to get back to sport and exercise, increasing your intake of certain macro and micro-nutrients and adopting an optimal loading approach will optimize tissue healing and recovery rates.
Stay Tuned for How to Eat Right to Decrease Low Grade Inflammation
[wdi_feed id=”1″]

